FES Electrode Placements for Upper Limb Stroke Recovery Vol.3
Shoulder
August 15, 2025
The shoulder plays a critical role in upper limb function, from stabilising the arm during fine motor tasks to enabling large movements like reaching or lifting. In post-stroke rehabilitation, shoulder dysfunction is common, often including weakness, abnormal tone, and instability. This volume of our FES placement series focuses on electrode positioning for shoulder activation, targeting specific muscles to support recovery and improve functional movement.
*All anatomical references and photographs in this guide are taken using the right arm for consistency.
1. Shoulder Extension
Purpose: Pulling objects backwards, propelling a wheelchair, stabilising in closed-chain movements.
Target Muscles:
Posterior deltoid
Latissimus dorsi
Teres major
Placement: Place one electrode over the posterior deltoid and the second over the latissimus dorsi (mid-axillary line, just below the scapula).
This FES can be combined with elbow extension (and even wrist extension) to simulate functional movements such as pushing open a door or propelling up from a chair armrest. Because shoulder extensors are not commonly hypertonic, spasticity is less of a concern. Incorporate extension stimulation into active therapy: for example, have the patient reach back to a target or press down on a surface with the stimulated arm. This helps strengthen the motion and improves the carryover into daily activities.
2. Shoulder Flexion
Purpose: Reaching forward or overhead (e.g., reaching a shelf, dressing).
Target Muscles:
Anterior Deltoid
Middle Deltoid
Placement: Place one electrode over the anterior deltoid belly and the other over the middle deltoid. Slight adjustments in placement (more medial toward the clavicle or lateral toward the deltoid tubercle) may be necessary based on patient anatomy to get a strong forward lift without recruiting the upper trapezius or pectoral muscles. If shoulder flexion is weak and the patient tends to bend the elbow or recruit biceps, consider using a second channel on the triceps to counteract the flexor synergy. Stimulating both the shoulder flexors and the elbow extensors simultaneously has been shown to produce more effective reaching movement in some post-stroke patients.
Integrate shoulder flexion FES into forward-reaching tasks such as reaching to touch a target or turn a light switch. This task-oriented approach helps the patient associate the stimulated movement with a functional goal, reinforcing voluntary control alongside the FES assistance.
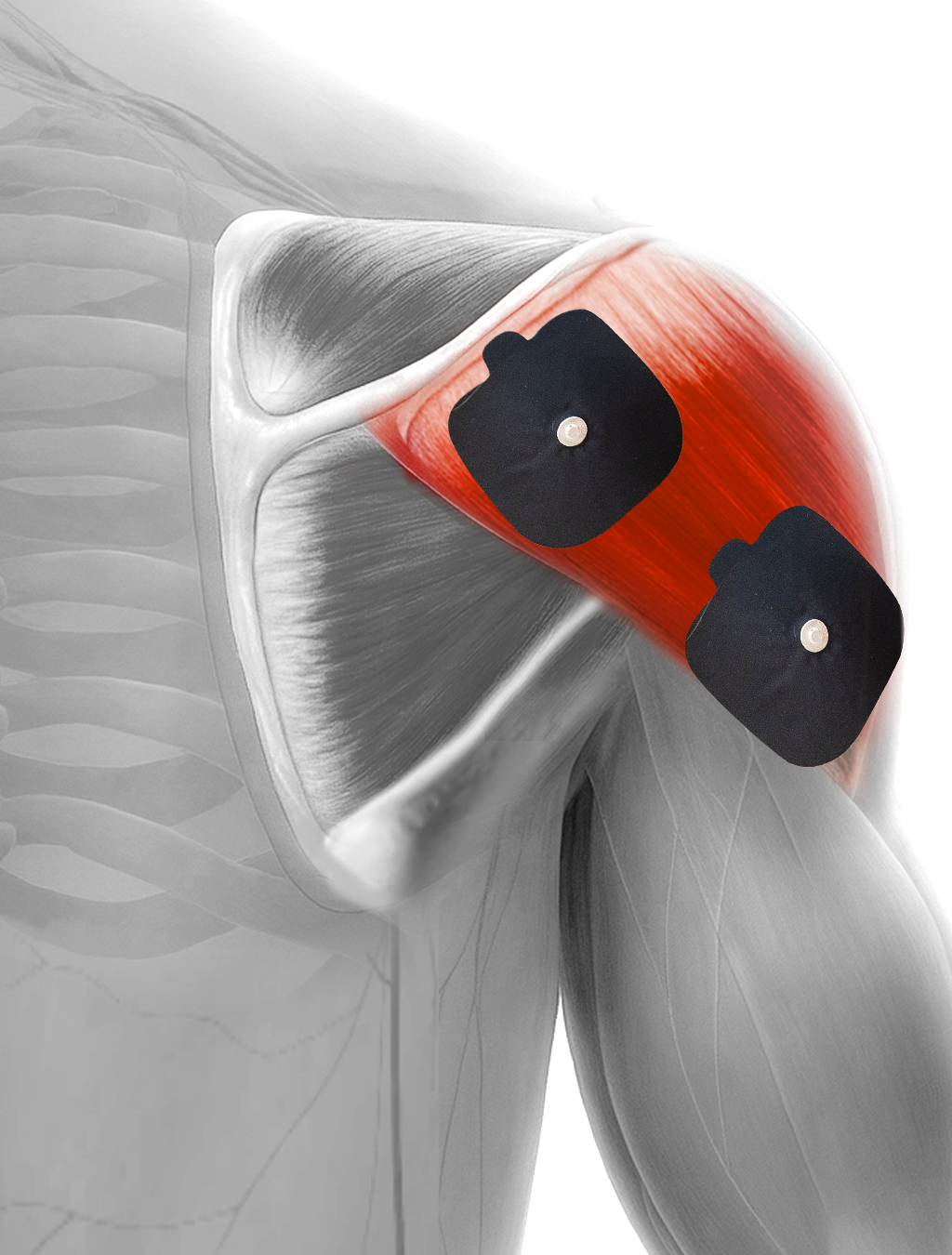
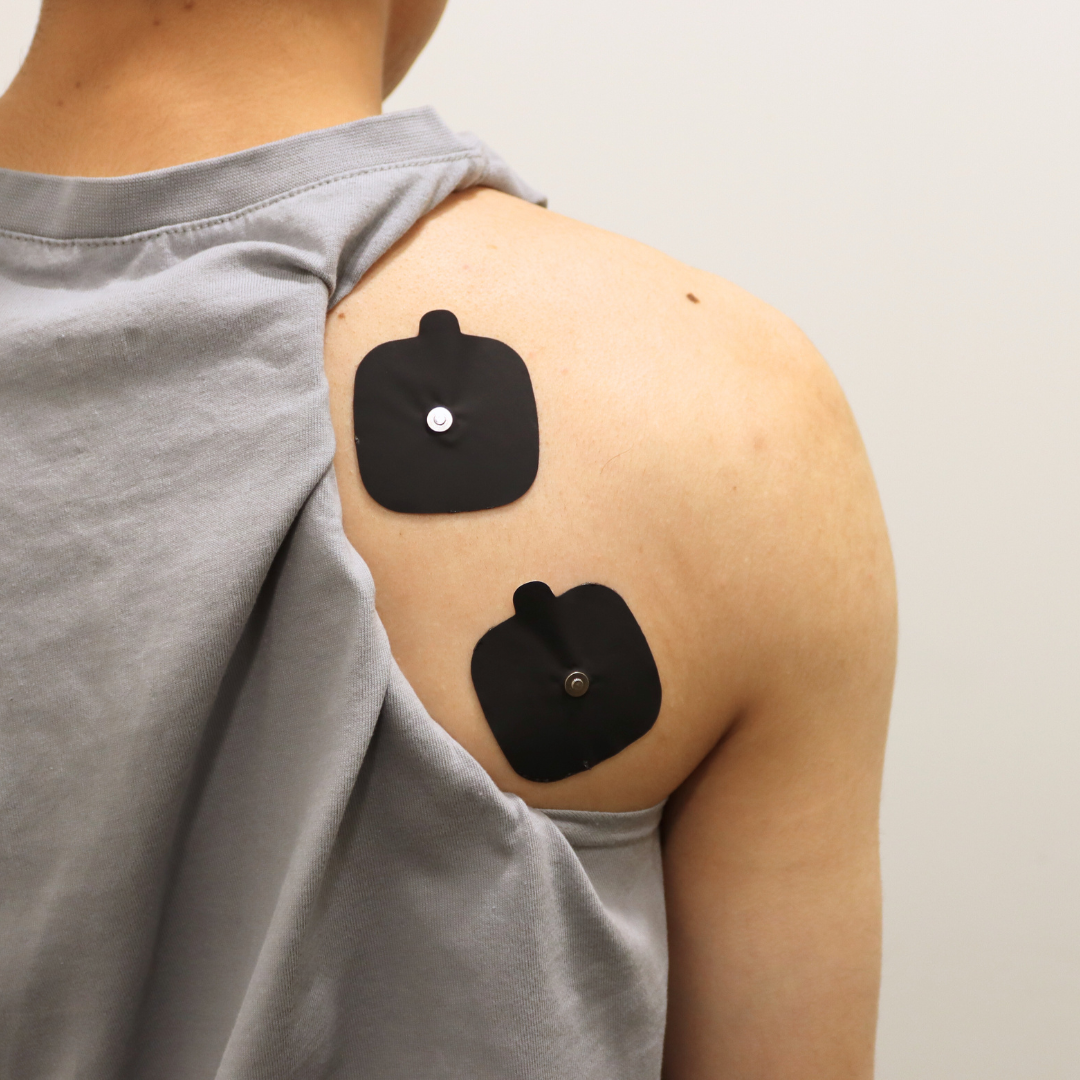
3. Shoulder Abduction
Purpose: Improve lateral reaching and help manage shoulder subluxation.
Target Muscles:
Middle Deltoid
Supraspinatus
Placement: Place one electrode over the belly of the middle deltoid. The second electrode is placed near the posterior deltoid or acromion.
If you notice excessive elevation or abduction, try a longer ramp-up time (≥2 seconds) to elicit a smoother contraction and reduce any spastic reflex in opposing muscles.
In practice, shoulder abduction FES can be paired with a second channel (e.g. stimulating external rotators or triceps) to promote a more natural reaching synergy.
Monitor closely to avoid compensatory trunk lean or shoulder hitching; adjust electrode placement if needed to achieve a pain-free abduction motion.
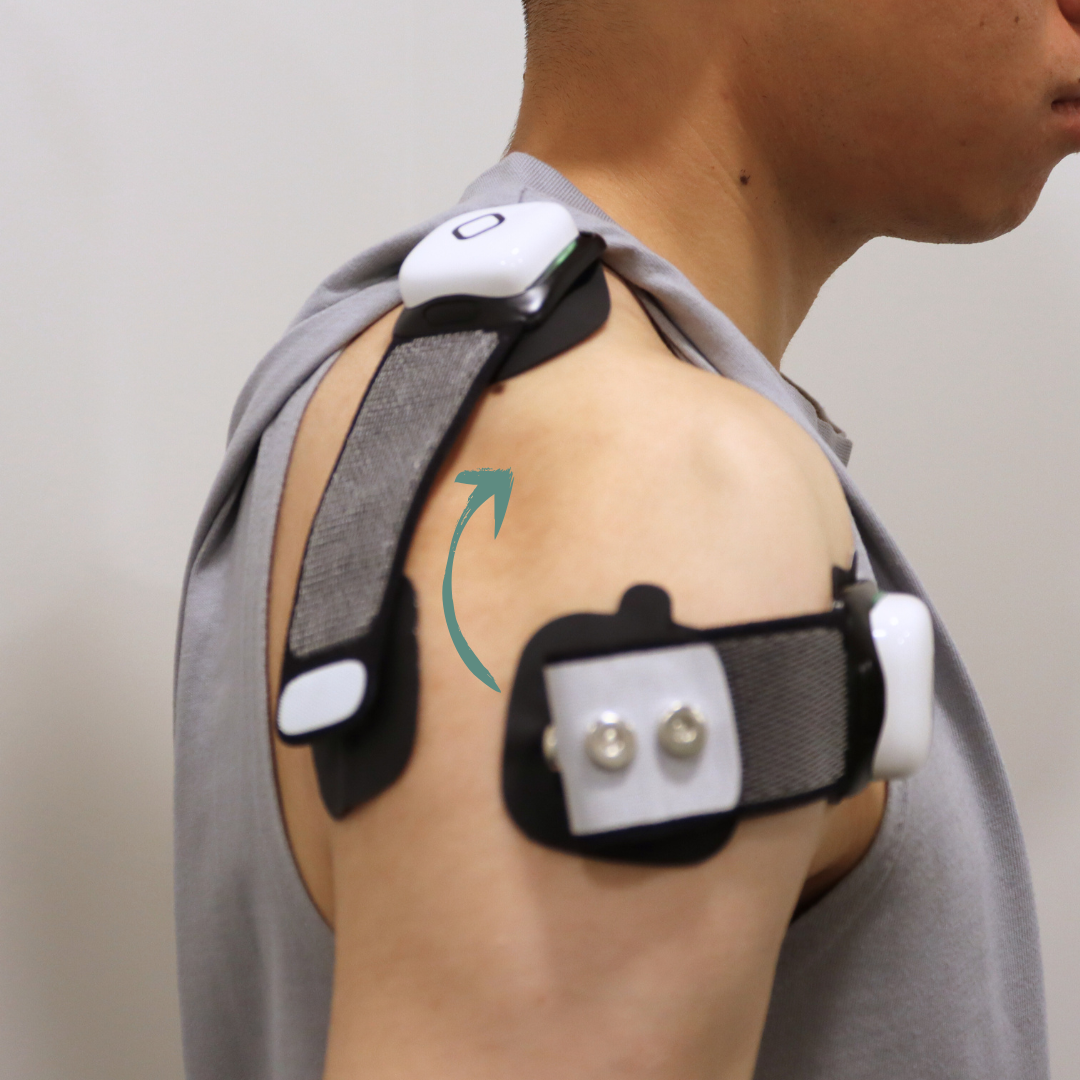
4. Shoulder Subluxation
Purpose: Reduce inferior displacement of the humeral head in early post-stroke recovery.
Target Muscles:
Supraspinatus
Deltoid (anterior/middle)
Placement: Use two channels (four electrodes). One channel’s electrodes are over the supraspinatus (on the upper shoulder, just above the scapula spine) and the middle deltoid, and the second channel’s electrodes are on the anterior and posterior deltoid. This combined stimulation lifts the humeral head into the glenoid fossa from multiple angles, promoting alignment without excessive shoulder abduction. Avoid upper trapezius activation. Pad placement should be adjusted so that you feel the humeral head elevate without a big shoulder shrug.
Use a slow ramp-up (at least 2 seconds) to avoid a quick jerk that could provoke spastic shoulder muscles or discomfort.
Clinical evidence strongly supports early and intensive use of FES for preventing shoulder subluxation in acute stroke.
Research suggests applying FES for a minimum of 1 hour daily, building up to ~6 hours per day over weeks, to significantly reduce subluxation risk and improve shoulder stability.
Combine the stimulation with functional training: for example, during active assisted shoulder exercises or while the patient practices supported weight-bearing through the arm.
5. Internal Rotation
Purpose: Bringing the arm toward the body (e.g., tucking in a shirt, fastening a seatbelt).
Target Muscles:
Subscapularis
Pectoralis major (sternal head)
Latissimus dorsi.
Placement: Place one electrode over the pectoralis major (sternal portion) and the other over the subscapularis region (anterior axilla).
Many stroke patients already dominate internal rotation due to spasticity of these muscles, use FES purposefully, typically to strengthen the motion for a specific functional goal (like tucking in a shirt or hooking a bra strap) once tone is under control. This contextual use helps the patient gain active control in tandem with the stimulation, rather than reinforcing any maladaptive pattern.
Emphasise proper posture: the scapula should be stabilised (avoiding excessive protraction) so that the internal rotators can work on turning the humerus, not yanking the shoulder blade.
Ensure that internal rotation FES is pain-free and does not trigger increased tone. A slow ramp and moderate intensity are key.
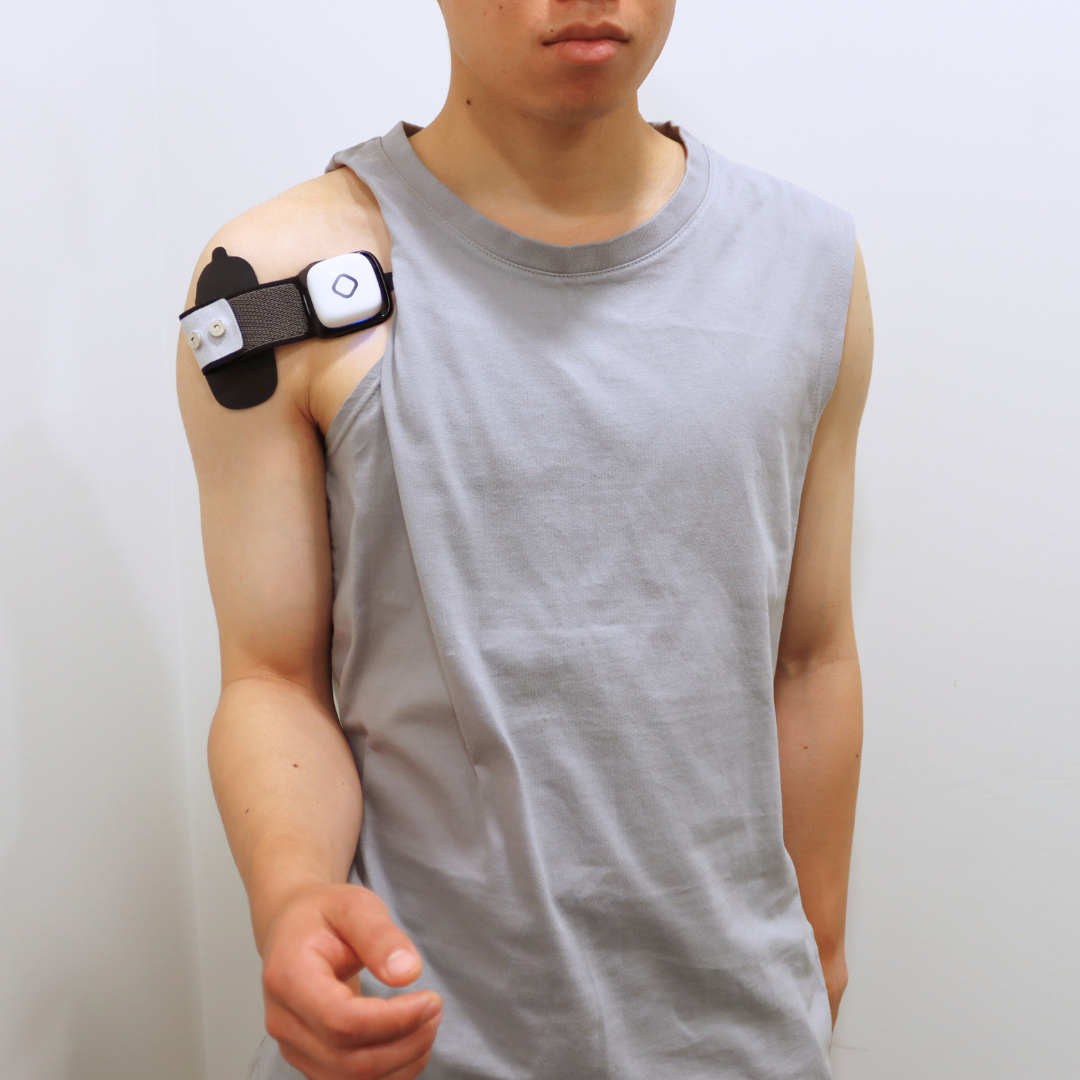
6. External Rotation
Purpose: Preparing the arm for reaching outwards, functional positioning for hand use.
Target Muscles:
Infraspinatus
Teres minor
Placement: Place one electrode over the infraspinatus (below the spine of the scapula) and the other over the teres minor (lateral border of the scapula, near the axilla). Small electrodes are often best for shoulder external rotators, as these muscles are small and lie under the deltoid.
Encourage the patient to incorporate FES-assisted external rotation into activities such as reaching out to shake someone’s hand, turning a doorknob/key, or tasks that require the arm to roll outward.
Clinically, activating the external rotators has the added benefit of promoting a more normalised movement pattern (it helps open up the chest and align the arm for reaching). Over time, this can diminish pain and impingement caused by the internal rotation posture.
Consistency is key: regular FES sessions for external rotation (even if brief) can yield improvements in active range and help inhibit the tone of the internal rotators during daily activities, thereby improving overall shoulder mechanics in the stroke-affected arm.
The shoulder is a complex joint, and its recovery after a stroke requires careful attention to both stability and mobility. FES can play a key role in retraining shoulder muscles, reducing subluxation, and supporting functional movement. The electrode placement, pad size, and stimulation parameters should be tailored to the individual. Combining FES with active participation and task-specific exercises helps the brain and muscles relearn how to work together, improving carryover into daily life.