FES Electrode Placements for Upper Limb Stroke Recovery Vol.1
Elbow, Forearm, Wrist
July 29, 2025
Functional Electrical Stimulation (FES) is an evidence-backed therapy for upper limb stroke rehabilitation, helping to strengthen weakened muscles, improve range of motion, reduce spasticity, and enhance motor control. It works by using surface electrodes to deliver electrical current to target muscles, eliciting contractions that facilitate movement in a paralysed or weak limb. However, correct electrode placement is critical. Placing the pads in the optimal positions ensures the intended muscle is stimulated and produces a smooth, functional movement. This guide (Volume 1 of a series) provides an accessible, educational overview of electrode placements for upper-limb movements (elbow extension/flexion, forearm supination/pronation, and wrist extension/flexion). Below, each movement is described with specific electrode placement tips and considerations.
*All anatomical references, illustrations, and example photos in this article depict the right upper limb (R arm) for consistency.
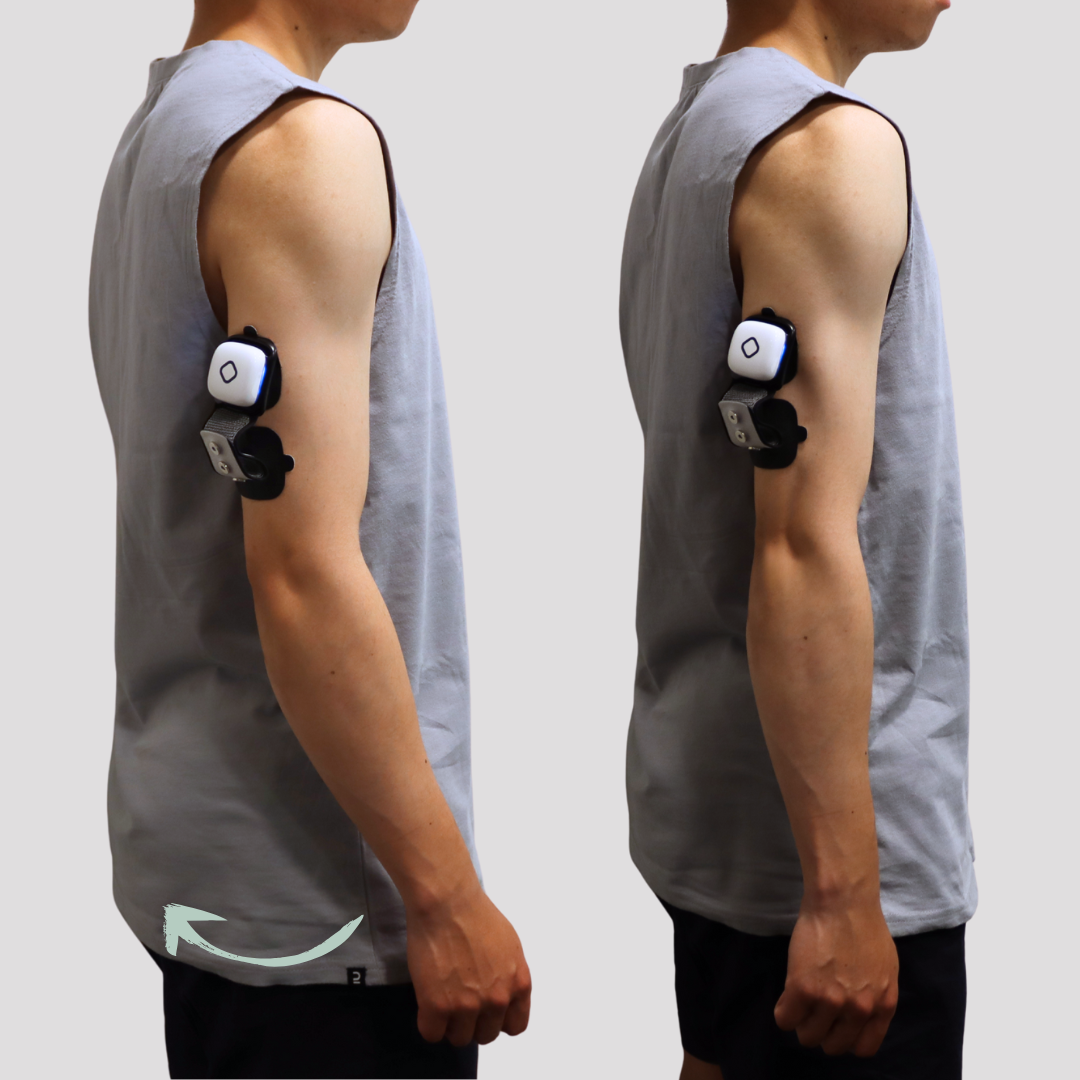
1. Elbow Extension
Elbow extension is often challenging for stroke survivors due to weakness of the triceps and dominant flexor synergies that make straightening the arm difficult. FES can be used to stimulate the triceps brachii and assist in extending the elbow, which is important for reaching and weight-bearing through the arm.
Posterior View - R Arm
For elbow extension, one electrode should be placed over the mid-belly of the triceps (on the back of the upper arm), corresponding to the motor point of the triceps muscle, and the other electrode is placed near the distal triceps tendon just above the elbow’s bony tip.
In practice, this means one electrode is roughly centred on the posterior upper arm, and the another one lies closer to the elbow joint on the triceps tendon insertion area. This placement will recruit the triceps to straighten the elbow; you will observe the forearm extending fully when stimulation is applied.
Functionally, restoring elbow extension helps with reaching out to grasp objects, pushing up from a chair, or stabilising the arm during activities. Therapists should start with a low intensity and gradually increase until the patient achieves a smooth extension without undue discomfort. Because stroke patients often have involuntary elbow flexor tension, activating the triceps via FES not only improves extension strength but can also help reduce abnormal flexor tone through reciprocal inhibition (engaging the triceps can relax the biceps). This placement is a foundational step in retraining more normalised reaching movements in stroke rehabilitation.
2. Elbow Flexion
Many stroke survivors already have a tendency for elbow flexor hyperactivity (flexor synergy), so FES for elbow flexion is often used when the biceps is weak or to improve coordination rather than strength alone. Proper placement and dosing can help activate the biceps without excessively facilitating any pathological flexor synergy.
Anterior View - R Arm
For elbow flexion, the biceps brachii is the primary target. One electrode is placed on the mid-belly of the biceps brachii over the belly of the biceps muscle, and the other electrode is placed near the lower end of the biceps, just above the elbow crease. This configuration effectively stimulates a biceps contraction to bend the elbow.
Functionally, this helps the patient bring the hand towards the face or chest, useful for activities like feeding or grooming.
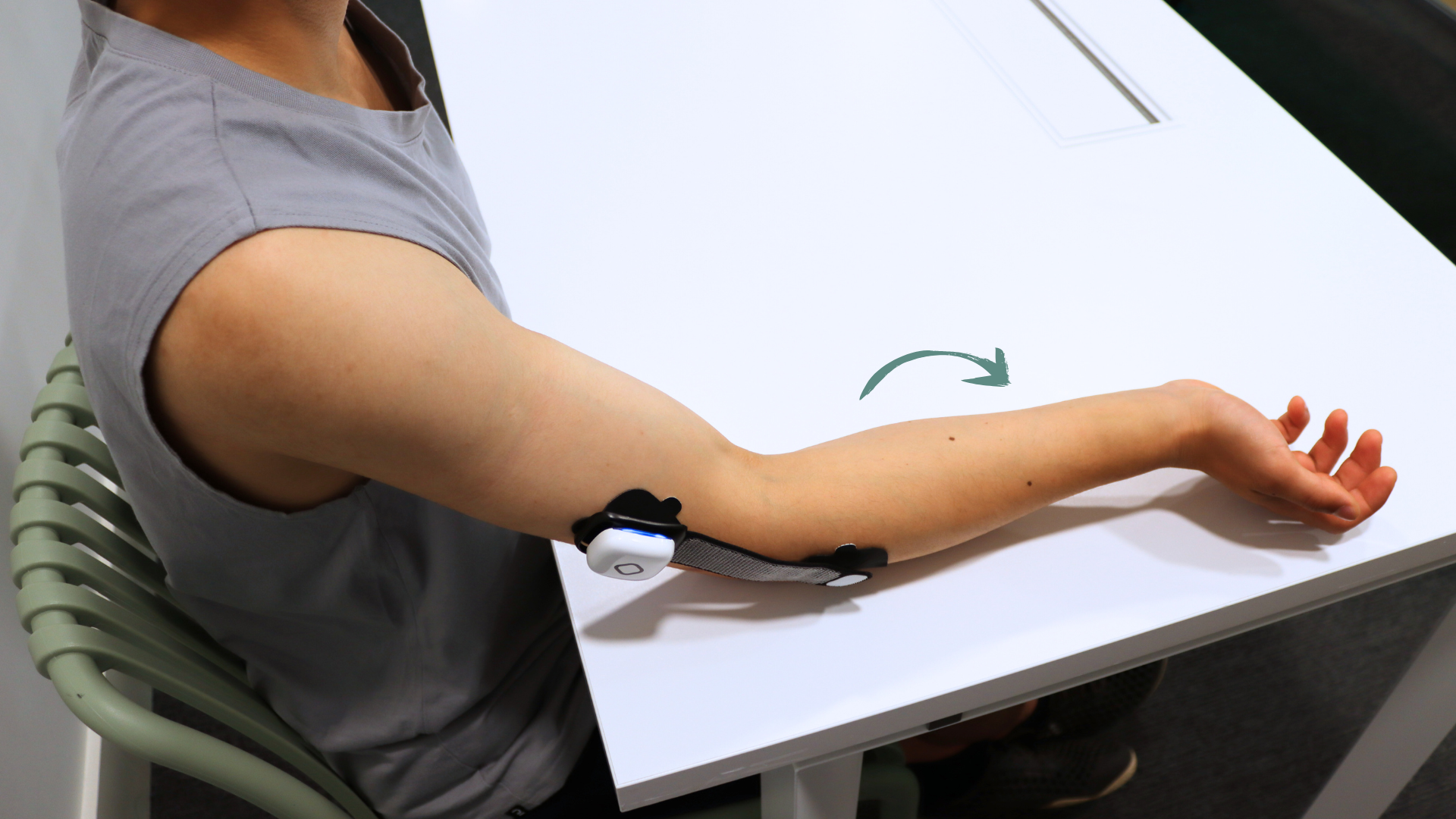
3. Forearm Supination
Supination (rotating the forearm so the palm faces upward) is a movement frequently impaired after stroke. Patients may struggle to turn their palms up to accept objects or perform tasks like feeding. The supinator muscle (and to some extent the biceps, which also assists in supination) is targeted with FES to improve this motion.
Place the first electrode very high on the dorsal-lateral forearm, just below the elbow near the lateral epicondyle (the bony outer part of the elbow). The second electrode is placed on the upper arm (above the elbow, over the triceps or near the shoulder). This arrangement creates a current pathway running longitudinally from the forearm into the upper arm.
Clinically, this placement causes forearm supination accompanied by some extension at the wrist and elbow (and even slight finger extension), because the current may also recruit the extensor muscles and triceps. This can be useful if the goal is to incorporate supination into a broader extensor synergy (for example, turning the palm up while also straightening the arm). If using this option, be mindful of the elbow and wrist movement: ensure it aligns with therapy goals (some therapists use it to encourage an “opening-up” pattern of the limb, which can counteract flexor synergy patterns).
Functionally, improving supination can greatly enhance a patient’s ability to carry objects with their palm up (like holding a bowl or carrying a tray) and perform personal care tasks that require palm-up orientation. Since supination is often coupled with shoulder and wrist movements, therapists may incorporate these electrode placements into task-specific training (e.g., supinating the forearm while reaching to pick up an object).
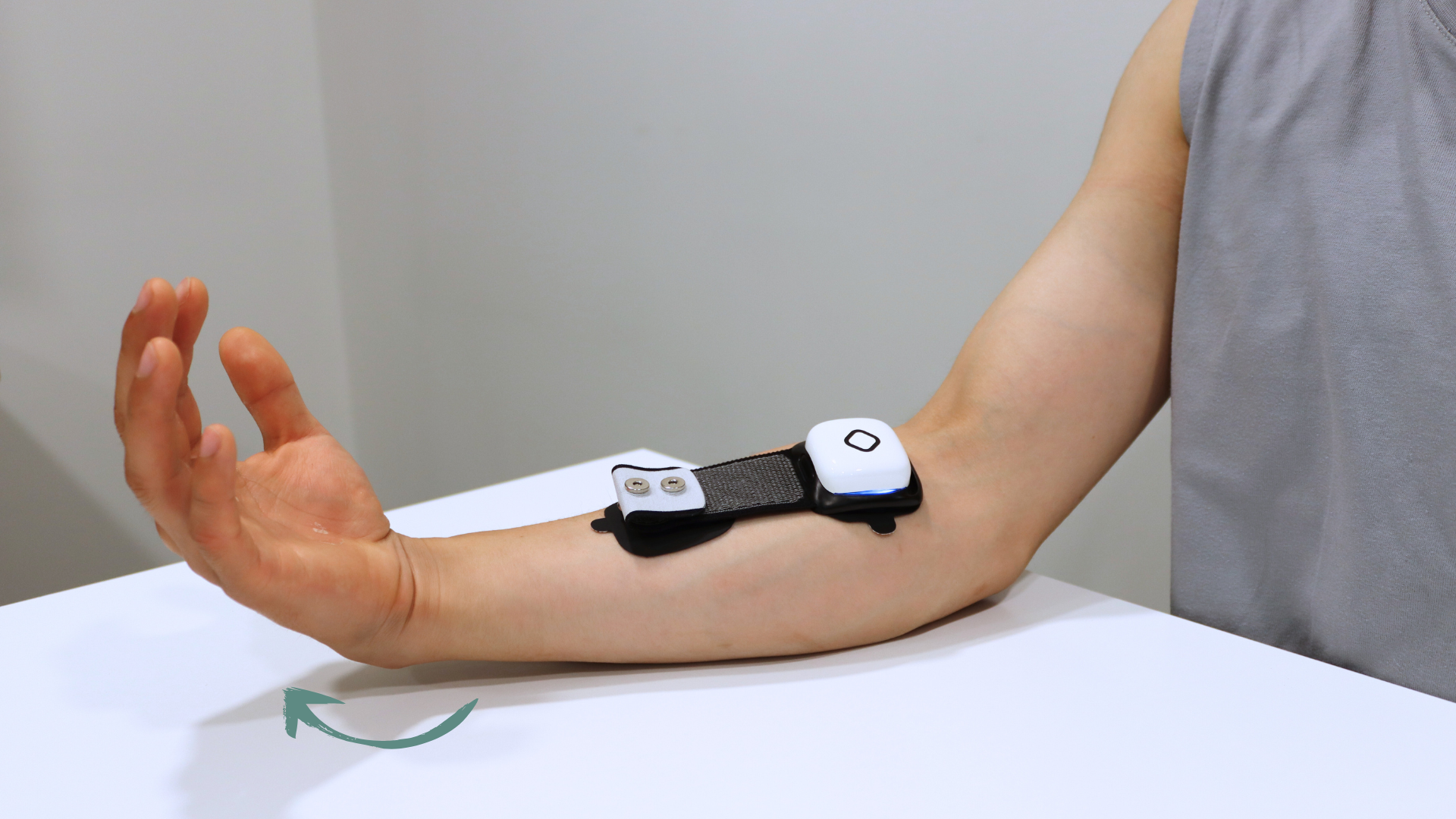
4. Forearm Pronation
Pronation (turning the palm downward) is another crucial movement, for example, when typing on a keyboard, grasping objects with the palm down, or using tools. After a stroke, some patients have difficulty pronating the forearm (especially if supinator and biceps tightness keep the forearm in a supinated or neutral position). FES can activate the pronator teres (the main superficial pronator muscle) to facilitate forearm pronation.
The first electrode goes on the proximal volar forearm, just below the elbow crease on the inner (ulnar) side, specifically between the midline of the forearm and the medial epicondyle of the humerus. This means placing the pad on the fleshy area about an inch or two distal to the medial elbow bone, toward the centre of the inner forearm. The second electrode is placed on the opposite side of the forearm, along the radial (thumb-side) border of the proximal forearm. With this arrangement, the electrical current passes through the upper forearm, stimulating the pronator teres, which runs from the inner elbow across to the outer radius.
Often, you will observe pronation coupled with a bit of wrist flexion. This co-contraction happens because the median nerve innervates both the pronator teres and some wrist/finger flexors, so the stimulation may also recruit the flexor muscles. If excessive wrist/finger flexion is occurring, the electrode positions might be adjusted slightly to focus more on the pronator teres (for instance, moving the pads to ensure they’re not too far distal where they would hit wrist flexors more directly).
Functionally, restoring active pronation allows stroke survivors to place their hand properly for tasks like writing, picking up objects from a table, or pressing down on surfaces. Therapists may train pronation by combining this FES setup with functional practice (e.g., turning a jar lid or using a screwdriver motion). As always, begin with low stimulation and watch for the desired rotation; correct placement will produce a clear turning of the forearm without excessive elbow or shoulder substitution.
5. Wrist Extension
Wrist extension is a critical movement for hand function. It enables an open hand posture and provides a stable base for grasp. Many stroke survivors have weakness in the wrist and finger extensors (due to extensor muscle paresis and/or overpowering flexor spasticity), resulting in a flexed, drooping wrist that impairs their ability to release objects or bear weight on the hand.
The targeted muscles are the extensor muscle group in the forearm (primarily the extensor digitorum and extensor carpi radialis longus/brevis). Typically, one electrode is placed on the dorsal forearm about 2–3 finger-breadths below the lateral epicondyle of the elbow. This spot corresponds to the motor point of the common wrist and finger extensors, roughly at the proximal third of the forearm. The second electrode is positioned further down the dorsal forearm, over the tendinous portion of those same extensor muscles, just proximal to the wrist joint. This longitudinal placement over the extensor mass ensures a strong contraction that pulls the wrist up. Minimal finger involvement is ideal because we often want to practice wrist extension in isolation or as part of opening the hand, without triggering a full finger extension reflex that could cause finger hyperextension. If finger or elbow movement is too pronounced, you may need to fine-tune electrode placement or intensity.
Clinically, FES-assisted wrist extension helps the patient achieve the functional dorsal wrist stability needed for tasks like releasing objects (since the wrist must extend to open the hand) and weight-bearing through an extended wrist (as in pushing up from a surface or supporting oneself with an outstretched arm). Over time, repeated stimulation of the wrist extensors can also help reduce flexor tightness by promoting muscle balance around the wrist. Make sure to monitor for muscle fatigue and adjust parameters (pulse width, frequency) to achieve a smooth extension without rapid fatigue. This placement is commonly demonstrated in stroke rehab protocols and is one of the fundamental FES setups for upper limb re-education.
6. Wrist Flexion
The primary muscles involved in wrist flexion are the flexor carpi radialis and flexor carpi ulnaris (with assistance from palmaris longus). To stimulate wrist flexors, the electrode placement is essentially the mirror-opposite of the wrist extension setup: one electrode is placed on the volar side of the forearm, relatively high up toward the elbow – near the medial epicondyle (inner elbow bone) where the flexor muscles originate. Another electrode is then placed a bit further down on the forearm’s flexor surface, roughly mid-forearm, over the wrist flexor tendons. With correct placement and balanced parameters, you can achieve isolated wrist flexion without significant finger flexion. This is important because many stroke patients already have an issue with excessive finger flexor tone; we want to activate the wrist flexors without overly recruiting finger flexors. If you observe the fingers clenching tightly along with the wrist flexing, consider adjusting the electrode positions slightly (for example, moving the distal electrode a little more proximal or lateral) to reduce direct stimulation of finger flexor muscles.
In terms of functional benefit, improving wrist flexion strength and control can aid in tasks like squeezing a soft object, bringing the palm to grasp a handle, or stabilising the wrist during activities that require a strong grip (wrist flexors co-activate during power grip).
This guide is intended to be an accessible educational resource, and we hope the outlined placements make it easier for practitioners to implement FES confidently. Proper electrode placement not only improves the efficacy of each stimulation session but also enhances patient safety and comfort, ultimately leading to better functional outcomes.